Electroneuromyography
Overview
Electroneuromyography (EMG) is an electrical recording of muscle activity that aids in the diagnosis of neuromuscular disease, which affects muscle and peripheral nerves.
Purpose
Muscles are stimulated by signals from nerve cells called motor neurons. This stimulation causes electrical activity in the muscle, which in turn causes contraction. A needle electrode inserted into the muscle and connected to a recording device detects this electrical activity. Together, the electrode and recorder are called an electromyography machine. EMG can determine whether a particular muscle is responding appropriately to stimulation, and whether a muscle remains inactive when not stimulated.
EMG is performed most often to help diagnose different diseases causing weakness. Although EMG is a test of the motor system, it may help identify abnormalities of nerves or spinal nerve roots that may be associated with pain or numbness. Other symptoms for which EMG may be useful include atrophy, stiffness, fasciculation (muscle twitching), cramp, deformity, and spasticity. EMG results can help determine whether symptoms are due to a muscle disease or a neurological disorder, and, when combined with clinical findings, usually allow a confident diagnosis.
EMG can help diagnose many muscle and nerve disorders, including:
- Muscular dystrophy
- Congenital myopathies
- Mitochondrial myopathies
- Metabolic myopathies
- Myotonias
- Peripheral neuropathies
- Radiculopathies
- Nerve lesions
- Amyotrophic lateral sclerosis
- Polio
- Spinal muscular atrophy
- Guillain-Barré syndrome ataxias
- Myasthenias
- Inflammatory myopathies
Precautions
No special precautions are needed for this test. Persons with a history of bleeding disorder should consult with their treating physician before the test. If a muscle biopsy is planned as part of the diagnostic workup, EMG should not be performed at the same site, as it may affect the microscopic appearance of the muscle. Also, persons on blood thinners should relay this information to the physician performing the EMG.
Description
During an EMG test, a fine needle is inserted into the muscle to be tested. This may cause some discomfort, similar to that of an injection. Recordings are made while the muscle is at rest, and then during the contraction. The person performing the test may move the limb being tested, and direct the patient to move it with various levels of force. The needle may be repositioned in the same muscle for further recording. Other muscles may be tested as well. A typical session lasts from 30–60 minutes, with individual muscles usually studied for a period of two to five minutes.
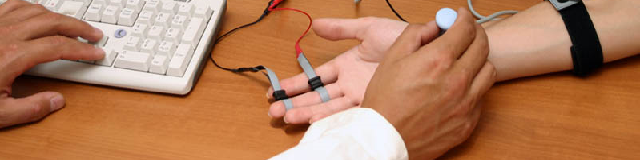
A slightly different test, the "nerve conduction velocity test," is often performed at the same time with the same equipment. In this test, stimulating and recording electrodes are used and small electrical shocks are applied to measure the ability of the nerve to conduct electrical signals. This test may cause mild tingling and discomfort similar to a mild shock from static electricity. Evoked potentials may also be performed for additional diagnostic information. Nerve conduction velocity and evoked potential testing are especially helpful when pain or sensory complaints are more problematic than weakness.
Preparation
No special preparation is needed. The doctor supervising and interpreting the test should be given information about the symptoms, medical conditions, suspected diagnosis, neuroimaging studies, and other test results.
Aftercare
Minor pain and bleeding may continue for several hours after the test. The muscle may be tender for a day or two.
Risks
There are no significant risks to this test, other than those associated with any needle insertion (pain, bleeding, bruising, or infection).
Normal results
There should be some brief EMG activity during needle insertion. This activity may be increased in diseases of the nerve and decreased in long-standing muscle disorders in which muscle tissue is replaced by fibrous tissue or fat. Muscle tissue normally shows no EMG activity when at rest or when moved passively by the examiner. When the patient actively contracts the muscle, spikes (motor unit action potentials) should appear on the recording screen, reflecting the electrical activity within. As the muscle is contracted more forcefully, more groups of muscle fibers are recruited or activated, causing more EMG activity.
The interpretation of EMG results is not a simple matter, requiring analysis of the onset, duration, amplitude, and other characteristics of the spike patterns.
Electrical activity at rest is abnormal; the particular pattern of firing may indicate denervation (for example, a nerve lesion, radiculopathy, or lower motor neuron degeneration), myotonia, or inflammatory myopathy.
Decreases in the amplitude and duration of spikes are associated with muscle diseases, which also show faster recruitment of other muscle fibers to compensate for weakness. Increases in the amplitude and duration of the spikes are typical of nerve diseases in which some degree of reinnervation (repair by new nerve connections to muscle) has occurred. Recruitment is reduced in nerve disorders.
Needle (Local) EMG
- Registration and analysis of spontaneous activity phenomena, calculation of potentials average frequency.
- Detection of motor unit potentials (MUP) in semiautomatic and manual modes.
- Automatic analysis of MUP parameters, determination of denervation-reinnervation process stageturn-amplitude and frequency analysis of interference curve.
Stimulation EMG
- Registration and analysis of M-wave characteristics and sensory action potential evaluation of motor/sensory conduction velocity
- F-wave, H-reflex (also including paired stimulation), T-reflex and blink reflex parameters study magnetic stimulation of spinal roots and peripheral nerves with the further classic analysis of motor response.
- Registration and analysis of GSR parameters.